A Practical Guide for Clinicians to manage Depression and Anxiety
A practical guide to managing depression and anxiety in the community setting.
Author: Dr. Jonathan Wee
Version: 1.0
Updated: 04/11/2021
Audience: GP, Medical Student
Subspecialty: Psychiatry
Conditions: Depression, Anxiety
Disclaimer: The author is sharing this information out of good will. As a clinician it is your responsibility to check the accuracy of the information before using it in your own clinical practice. This is also not a complete, definitive or expert guide. It is your responsibility to know the nuances of clinical assessment and management which are not explained in this guide.
- Step #1: Patient History Taking
- Step #2: Management of Patients
- 1. Explanation
- 2. Safety plan
- 3. Psychotherapy
- 4. Daily exercise
- 5. Sunlight exposure first thing in the morning
- 6. Fish oil supplement
- 7. Antidepressant use
- 8. Mindfulness meditation
- 9. Socialising
- 10. Scheduling hobbies
- 11. Online resources to explore
- Step #3: Further investigation into patient’s medical condition
Step #1: Patient History Taking
Here is my most efficient approach to getting the most important information out in a limited time.
Patients often only book in a single appointment for their mental health despite being told in advance that such a consult should ideally be done over a double appointment.
Types of questions to ask patients
- Tell me about your mental health
- When did this all start?
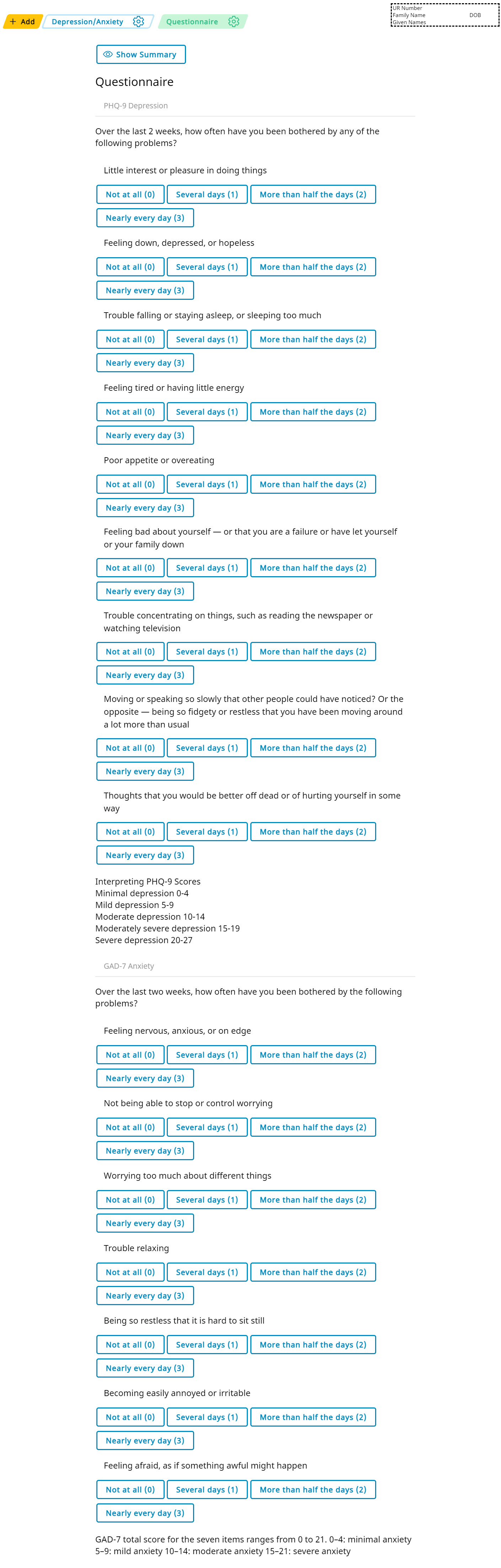
- PHQ-9 Questionnaire
- GAD-7 Questionnaire
- Do you drink much alcohol?
- Do you use any recreational drugs?
From the PHQ-9 Questionnaires and the GAD-7 Questionnaires, you can see if they meet the DSM-V Criteria for Depression or Anxiety. The questions in the PHQ-9 or GAD-7 pretty much match up with the DSM-V criteria between both questionnaries.
The PHQ-9 questionnaire can tell you if the patient has had thoughts of self harm or suicide. If they have suicidal thoughts, clarify if they have had thoughts recently, if they are thoughts or plans, and if they have acted on these thoughts in the past.
For Generalised Anxiety Disorder, the following relating features are found in the PHQ-9:
- being easily fatigued
- difficulty concentrating
If there isn’t enough to diagnose anxiety according to DSM-V, ask about muscle tension (this symptom is not covered by either PHQ-9 or GAD-7).
An example how I document their symptoms efficiently is as such:
PHQ-9 = 21 (3, 3, 2, 2, 3, 2, 2, 3, 1)
Patient meets criteria for clinical depression as per DSM-V
GAD7 = 18 (3, 3, 3, 2, 2, 2, 3)
Patient meets criteria for generalised anxiety disorder as per DSM-V
Step #2: Management of Patients
1. Explanation
Explain that they meet the diagnostic criteria for depression and/or anxiety based on their answers.
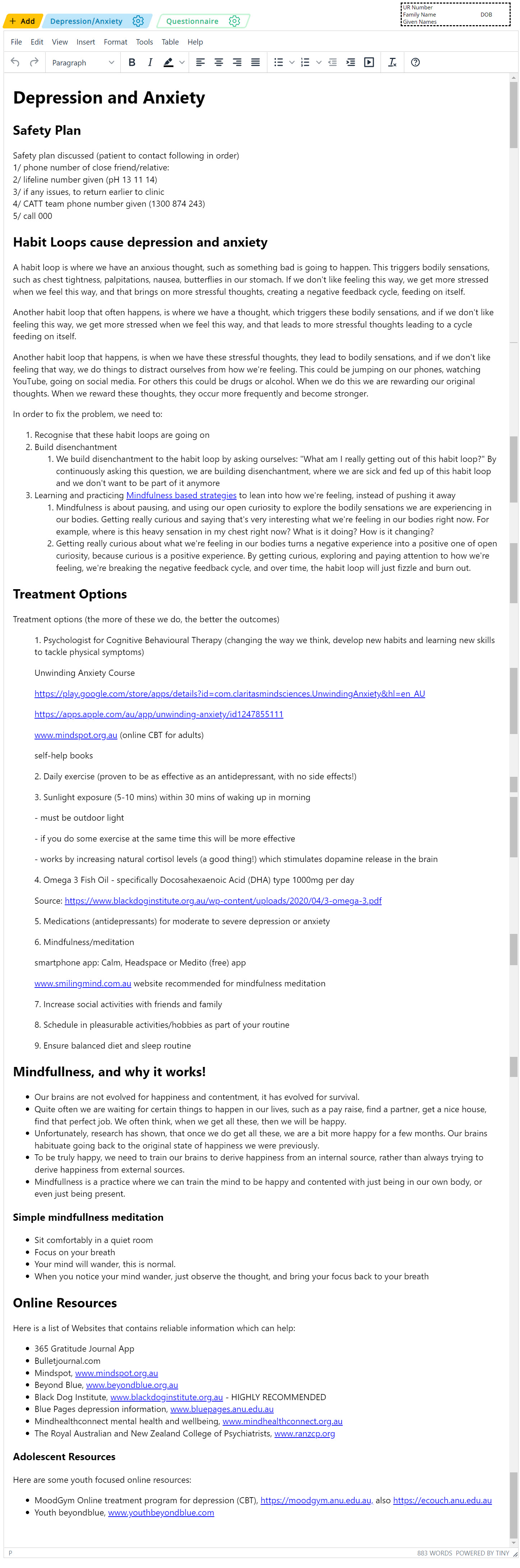
Habit Loops
Explain that the root cause of depression or anxiety is caused by habit loops.
A habit loop is where we have an anxious thought, such as something bad is going to happen. This triggers bodily sensations, such as chest tightness, palpitations, nausea, butterflies in our stomach. If we don’t like feeling this way, we get more stressed when we feel this way, and that brings on more stressful thoughts, creating a negative feedback cycle, feeding on itself.
Another habit loop that often happens, is where we have a thought, which triggers these bodily sensations, and if we don’t like feeling this way, we get more stressed when we feel this way, and that leads to more stressful thoughts leading to a cycle feeding on itself.
Another habit loop that happens, is when we have these stressful thoughts, they lead to bodily sensations, and if we don’t like feeling that way, we do things to distract ourselves from how we’re feeling. This could be jumping on our phones, watching YouTube, going on social media. For others this could be drugs or alcohol. When we do this we are rewarding our original thoughts. When we reward these thoughts, they occur more frequently and become stronger.
In order to fix the problem, we need to:
- Recognise that these habit loops are going on
- Build disenchantment
- We build disenchantment to the habit loop by asking ourselves: “What am I really getting out of this habit loop?” By continuously asking this question, we are building disenchantment, where we are sick and fed up of this habit loop and we don’t want to be part of it anymore
- Learning and practicing Mindfulness based strategies to lean into how we’re feeling, instead of pushing it away
- Mindfulness is about pausing, and using our open curiosity to explore the bodily sensations we are experiencing in our bodies. Getting really curious and saying that’s very interesting what we’re feeling in our bodies right now. For example, where is this heavy sensation in my chest right now? What is it doing? How is it changing?
- Getting really curious about what we’re feeling in our bodies turns a negative experience into a positive one of open curiosity, because curious is a positive experience. By getting curious, exploring and paying attention to how we’re feeling, we’re breaking the negative feedback cycle, and over time, the habit loop will just fizzle and burn out.
2. Safety plan
If the patient has suicidal thoughts or ideations, you must make a safety plan. Asking the patient who they would call over the phone if they need help or felt suicidal, and enter this in the safety plan. Having a list of 3 names is ideal. Explain that the safety plan is the order in which you would contact people for help. The number listed in the safety plan above is for the North Western Melbourne Psychiatric Crisis Assessment Team. Please change this number to the one of your local service.
3. Psychotherapy
Psychotherapy is the most important treatment option. It addresses the root cause of depression and anxiety. Most patients would also prefer to try this over medications as a starting point.
One option is to refer the patient to a psychologist. My preference is one that focuses primarily on Cognitive Behavioural Therapy. The benefit from a psychologist is that they can tailor therapy to the patient, and address their specific habit loops, cognitive biases and distorted thoughts.
Another option is online psychotherapy. For anxiety, the Unwinding Anxiety Course online mindfulness based cognitive behavioural therapy (CBT) course developed out of Brown University is an excellent 6 week course. It costs ~$50 per month, and your patient can cancel the subscription once they are done with the course. Another excellent course is the Mindspot Online Program, which is government funded and is free for the patient. They have a suite of courses which range from depression and anxiety, to obsessive compulsive disorder (OCD, post-traumatic disorder (PTSD) and chronic pain. The major benefit is that unlike psychotherapy with a psychologist, it engages the patient daily as opposed to a psychologist session every 2-4 weeks. It is the daily practice and daily habits where progress is truly made.
4. Daily exercise
Daily exercise has been proven to be just as effective as an antidepressant for depression and anxiety, with no side effects!
5. Sunlight exposure first thing in the morning
Patients who have depression and anxiety often have sleeping problems. Fixing insomnia is essential to fixing the mood disorder. Our brains rely on direct sunlight to train and strengthen our biological clock. Direct sunlight outdoors (40,000 lumens outdoors on a cloudy day vs 1000 lumens indoors) within 30 mins of waking stimulates a physiological cortisol spike which in turn stimulates natural dopamine release in the brain. This daily practice results in higher quality deep sleep at night time, and improves moods during the day.
6. Fish oil supplement
Taking 1000 mg DHA type omega 3 fish oil daily has been shown to be almost as effective as taking an antidepressant, with no side effects.
7. Antidepressant use
Antidepressants are recommended in conjunction with psychotherapy for moderate to severe depression or anxiety. You can tell from their PHQ-9 and GAD-7 scores their severity and recommend an antidepressant based on their score. When the patient is moderate to severe in severity, the benefits of an an antidepressant are likely to outweigh their risks and adverse side effects.
There are 2 ways to start an antidepressant:
- Pharmacogenomics blood test (PGx Mental Health)
- To order this blood test, write “PGx Mental Health” on a pathology form
- This test costs about $150 to do, and takes 2 weeks for the report to come back
- The blood test will list all the antidepressants and state one of the following options:
- The antidepressant will work as expected
- The antidepressant will have increased adverse reactions than expected
- The antidepressant may have no effect for the patient
- Start an antidepressant empirically (trial and error)
We are planning to create a template for discussing Escitalopram intiation with your patient, which will appear here shortly.
8. Mindfulness meditation
The Headspace App is very useful to patients to guide them through mindfulness meditation. Medito is a free app which is also good.
Doing a minimum of 8 mins of mindfulness meditation per day causes structural changes in the brain that are detectable on an MRI-scan, and is a powerful way to treat mood disorder. Mindfulness meditation works!
9. Socialising
Being socially isolated is toxic for our mental health. Some studies have shown that it is worse than smoking for our health. If the patient is socially isolated, encouraging them to think about ways to socialise more as part of their routine is very important for their mental health. If the patient has social anxiety disorder, encouraging them to socialise with people they feel comfortable with is a good start.
10. Scheduling hobbies
Often patients feel that they need their motivation back to be able to enjoy and do their hobbies. In fact, it’s the other way around. Patients need to start doing their hobbies, then their motivation will return. We can’t rely on a patient’s motivation to do their hobbies, as with depression they don’t have the motivation to do it. Instead, we need to encourage the patient to schedule their hobbies as part of of their daily routine, so they are not relying on their motivation to do it. This is called activity scheduling. Asking the patient to rate how they feel before and after doing the activity helps bring to their attention that doing it is helping improve their moods. Patients can download the myCompass app or use an activity record sheet to track their daily progress.
11. Online resources to explore
Letting the patient know a list of online resources to explore gives these links credibility, increasing the chance of a patient’s self agency in exploring resources and tools to help themselves.
Step #3: Further investigation into patient’s medical condition
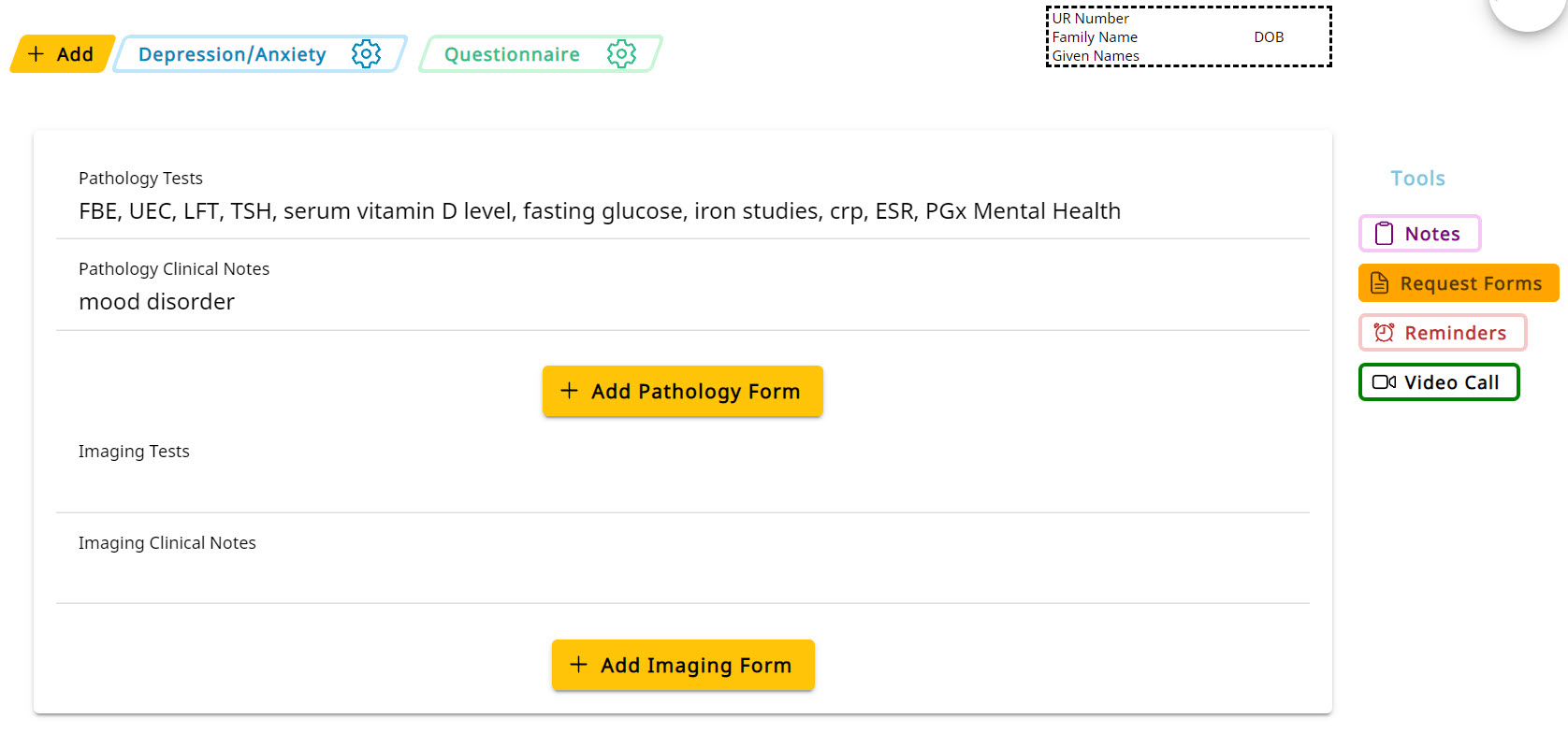
Pathology
If there is clinical suspicion of an underlying medical condition, the following blood tests may be useful. Personally I don’t always order these tests as the yield is generally low in the setting of mental health.
The tests I would order if I needed to rule out underlying organic medical cause are:
- FBE
- to exclude anaemia
- UEC
- to exclude organ failure
- LFT
- to exclude organ failure
- TSH
- to exclude hypothyroidism in the setting of depression, or hyperthyroidism in the setting of anxiety
- serum vitamin D level
- has been linked with mood disorder
- fasting glucose
- to exclude diabetes
- iron studies
- to exclude iron deficiency
- crp, ESR
- to exclude an underlying inflammatory disorder
- PGx Mental Health
- Pharmacogenomics DNA blood test which characterises the patient’s liver enzymes. This test typically costs $150 for the patient (no medicare rebate) and takes 2 weeks for a report to be completed. The report is able to outline which antidepressants should work as expected, which are likely to have no or minimal effect, and which are expected to have increased adverse effects.

Article by
Dr. Jonathan Wee
RACGP, MBBS, BBiomedSc; Co-Founder of HealthStencil
Jonathan is a practicing General Practitioner at MC Medical, Docklands, Victoria. He is also co-founder, web developer and designer for HealthStencil.
